Overview
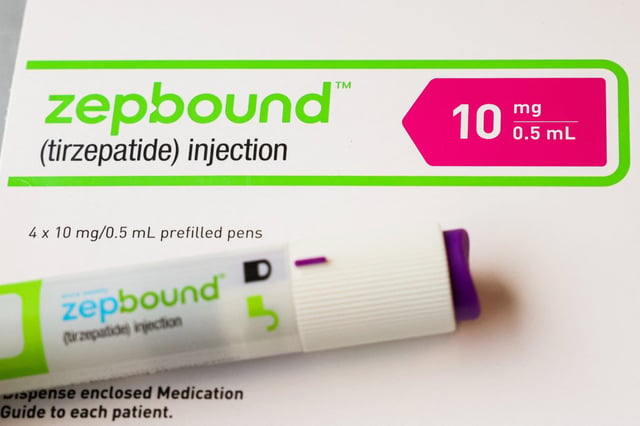
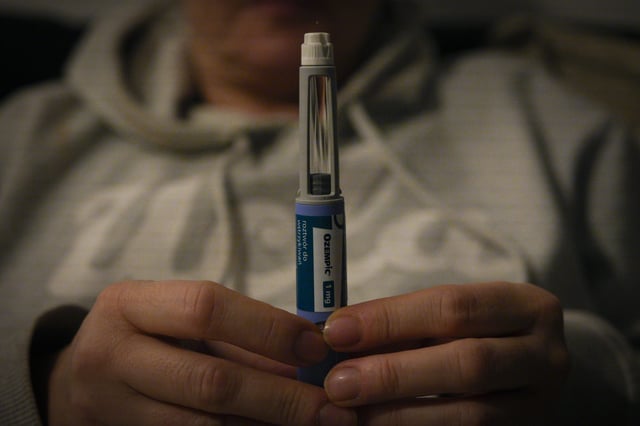
- New obesity drugs Wegovy and Zepbound are showing promising results but remain out of reach for millions of older Americans as Medicare is forbidden to cover such medications.
- Lawmakers are pushing to change a decades-old law that prohibits Medicare from paying for new weight loss drugs, arguing that the U.S. cannot afford to keep it in place as obesity rates rise among older adults.
- Research shows that the initial cost of covering these drugs could drain Medicare’s already shaky bank account, with a Vanderbilt University analysis estimating an annual price of about $26 billion if just 10% of Medicare’s enrollees were prescribed the medication.
- Other research suggests that covering the drugs could save the government billions, even trillions over many years, by reducing some of the chronic conditions and problems that stem from obesity.
- Pharmaceutical companies are preparing for a lobbying blitz next year to push for Medicare coverage of these drugs, with Novo Nordisk and Eli Lilly already spending millions on lobbying efforts.

![[Photo: Ketut Subiyanto/Pexels]](/cdn-cgi/image/onerror=redirect,width=640,height=640,format=webp/https://storage.googleapis.com/uploads.mongoosehq.com/url/media/6140469/e813dd87a3e02aaaf583001528ec325b963869c06a20bd3c49d3152bbb701e82)